While the Plan to End AIDS made important gains in the fight against HIV, it fell short of achieving a central and original goal of reducing estimated new HIV infections to 750 across New York State and 600 in New York City by 2020.
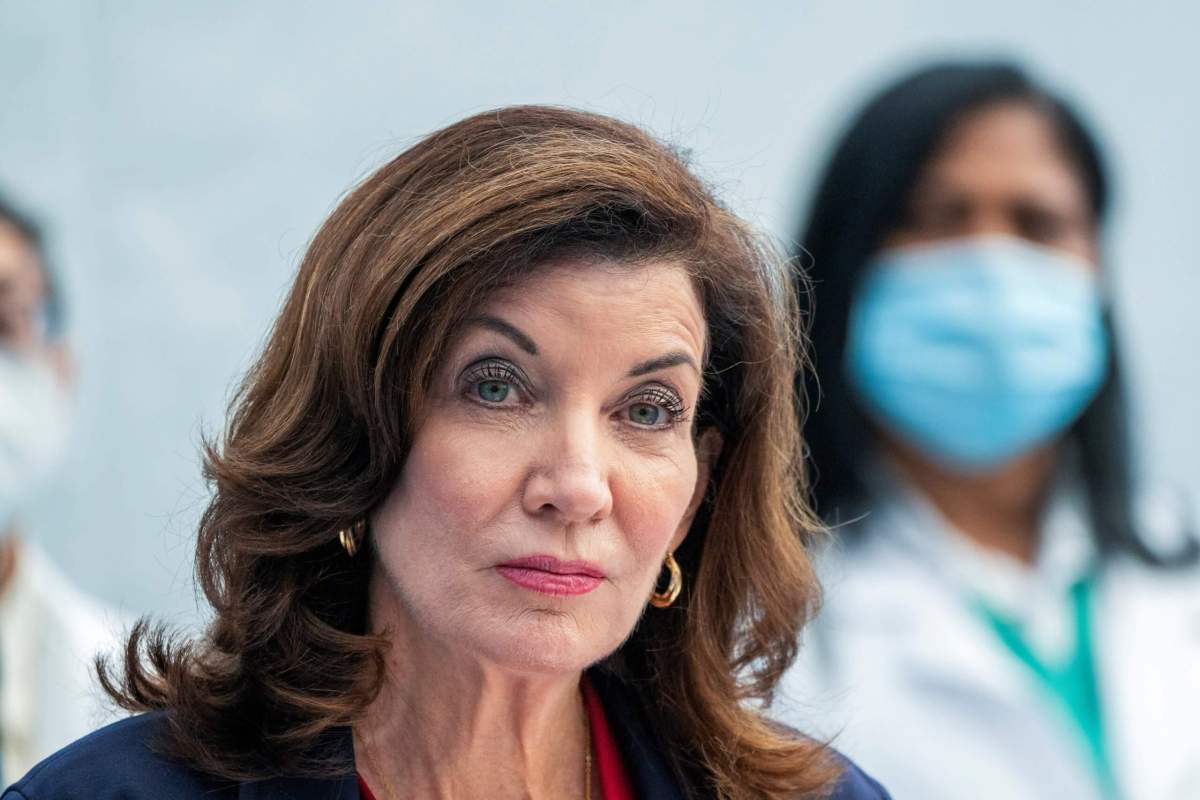
“This year’s Ending the Epidemic Summit is a time to reflect on both the progress we’ve made and the challenges we still face, and to reenergize our shared goal of ending the AIDS epidemic by 2024,” Governor Kathy Hochul said in a November 30 press release. In extending the timeline to 2024, the governor’s office cited the impact of the COVID-19 pandemic.
The governor’s press release reported that there were an estimated 1,467 new HIV infections statewide in 2020. A New York City health department HIV surveillance report that is released annually on December 1, World AIDS Day, reported that there were an estimated 1,200 new HIV infections in the city in 2020. While those estimates do show a continuing decline in new HIV infections, they remain well above the targets.
Launched in 2014, the Plan to End AIDS was conceived by Charles King, the chief executive of Housing Works, an HIV services organization, and Mark Harrington, the executive director of the Treatment Action Group, an advocacy organization.
King and Harrington envisioned moving people who are newly infected into treatment quickly to keep them healthy and to reduce the amount of HIV in their bodies to the point that they would be unable to infect others. The plan linked HIV-positive people to medical care and housing, nutrition, transportation, and other services. Those services make it easier for people to stay on their anti-HIV drugs.
The plan deployed pre-exposure prophylaxis (PrEP), which gives anti-HIV drugs to HIV-negative people to keep them from acquiring HIV, and post-exposure prophylaxis (PEP), which gives anti-HIV drugs to HIV-negative people with a recent exposure to the virus to keep them from becoming infected. Both drug regimens are highly effective when used correctly.
King marshalled support from HIV and health groups across the state. He won endorsements and money from Governor Andrew Cuomo, who resigned this year following credible allegations from multiple women that he had sexually harassed them, and Bill de Blasio, whose second and final term as New York City’s mayor will end on January 1.
The organizations engaged in the plan tracked their progress on a website that shows success on a number of goals. On some measures, the plan did not meet its targets, but still showed progress.
A major goal, and probably its most ambitious goal, was to reduce the number of estimated new HIV infections to 750 statewide in 2020. New HIV diagnoses could have occurred years before the diagnosis was made. Estimated new HIV infections are the gold standard. Since most new HIV infections in New York occur in New York City, the city adopted its own target of 600 estimated new HIV infections in 2020.
In 2019, government officials and activists were already conceding, at least tacitly, that they were unlikely to hit the numbers for estimated new HIV infections in 2020. In 2020, the new targets for that metric on the Ending the AIDS Epidemic dashboard were changed to 825 statewide and 660 in the city. In her November 30 statement, Hochul moved the target date to the end of 2024, giving the plan another three years to meet all of its goals. Those goals remain ambitious.
The new deadline gives the state three years to produce a 44 percent decline in new HIV infections. The city’s estimated 1,200 new HIV infections in 2020 require that it produce a 45 percent decline in estimated new HIV infections to achieve 660 new infections in three years. The HIV surveillance report shows that the city took from 2016 through the end of 2020, or five years, to reduce estimated new HIV infections from 1,700 to 1,200, a 29 percent decline.
The city reported that there were 1,396 new HIV diagnoses in New York City in 2020, with 1,091 occurring among men and 256 occurring among women. Forty-nine transgender people were newly diagnosed in 2020.
Forty-seven percent of the new HIV diagnoses in 2020, or 661, were among Black people; 474, or 34 percent, were among Latinx individuals; and 187 of the new HIV diagnoses, or 13 percent, were among white people. Sixty-four percent of the new diagnoses, or 893, occurred among people aged 20 to 39. In its press release, the city noted the disparities.
“Of all cisgender and transgender women newly diagnosed with HIV in 2020, 92% were Black or Latina, and of all cisgender and transgender men newly diagnosed, 79 percent were Black or Latino,” the press release read. “Of all men newly diagnosed with HIV in 2020, 59 percent were [men who have sex with men (MSM)]; of all new diagnoses among MSM, 78 percent were among Black or Latino MSM, 79 percent of whom were ages 20-39 years. And nearly half of New Yorkers newly diagnosed with HIV in 2020 lived in neighborhoods of high or very high poverty.”
The city has seen large declines among injection drug users due to the distribution of clean needles. In 2020, 12 new HIV diagnoses were attributed injection drug use with another 10 attributed to injection drug use among MSM. Mother-to-child transmission accounted for just two new HIV diagnoses. Where the city has failed is in delivering effective HIV prevention services to Black and Latinx gay and bisexual men.